Smplicare Ltd - Glasgow City Region
Alex Melling & Garrett Sprague
Smplicare’s AgeWell Coaching App uses real-time data and AI to assess fall risk, support self-management, and enhance falls prevention services for older adults through digital health integration.
Funded by the Department of Science Innovation and Technology (DSIT) as part of the 5GIR programme, Glasgow City Region (GCR) utilised circa £750,000 to develop an innovation scheme, ensuring rapid outcomes within an 8-month period across the 5G Glasgow City Region (GCR) between September 2004 and March 2025. As part of the Smart and Connected Social Places Program, the Smplicare innovation project aims to identify and predict fall risks to adults using real-time data.
Falls in older adults remain a major public health concern, driving high healthcare costs and loss of independence. This project piloted Smplicare’s AgeWell Coaching Platform and validated its Fall Risk Algorithm (SFRa) in real-world settings, advancing the tool from TRL 4 to TRL 6.
Over four months, 35 participants used the AgeWell App alongside Fitbit devices to track activity and sleep. Real-time fall risk scores were generated through the SFRa, while user feedback informed updates such as goal-setting features and new fall-prevention exercises.
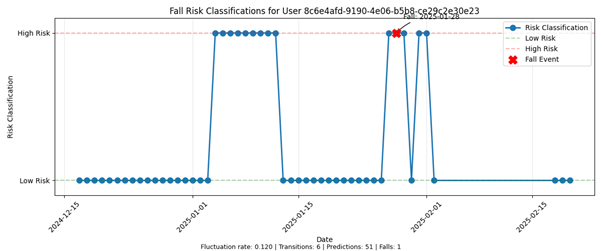
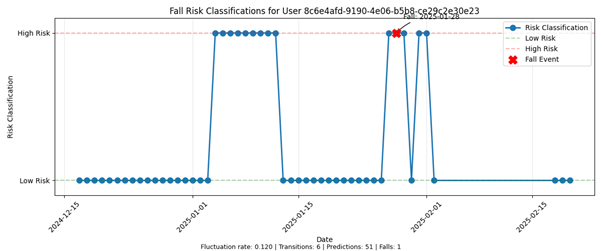
Results showed strong engagement, with 78.2% average Fitbit data compliance and 64% of users accessing the app at least three times a week. One fall incident aligned with a high-risk score, reinforcing the algorithm’s predictive potential.
Working with Later Life Training and falls teams in North and South Lanarkshire, the project explored how digital tools can complement existing prevention programmes. The pilot demonstrated that Smplicare’s platform is a scalable solution for enhancing falls prevention and self-management in older adults, with promising implications for broader public health and care services.
What is the Problem to be solved?
Falls among older adults are a major and growing public health issue. In the UK, 30% of adults over 65 fall each year, with 5% resulting in fractures or hospital admissions. Falls cost the NHS approximately £4.4 billion annually, while in Scotland alone, the system-wide cost was £470 million in 2013, projected to exceed £800 million by 2023/24. Fragility fractures alone account for £1.1 billion and 1.8 million hospital bed days annually.
This case study is aimed to support Health and Social Care Partnerships (HSCPs), local authorities, NHS falls prevention teams, housing associations, and care providers seeking scalable digital solutions to reduce falls among older adults living independently or semi-independently. It also informs decision-makers responsible for technology adoption and healthy ageing strategies across the public sector.
The Glasgow City Region faces disproportionate challenges:
- 18.3% increase in falls-related mortality since 2018
- Region responsible for 69% of Scotland’s increase in unintentional injury (UI) fall-related hospital bed days
- 5.1% rise in Emergency Department Admissions (while Scotland overall saw a 1.3% decrease)
- 15.5% rise in femur fractures in the region vs. 5.7% nationally
These figures highlight a clear and urgent need for scalable, accessible, and proactive fall prevention solutions.
Traditional strength and balance classes (e.g., FaME, Otago) are effective but face issues with:
- Long waiting lists
- Limited staffing and facility availability
- Inaccessibility for those who cannot travel
- High drop-off post-programme
Digital tools are underused, particularly among older adults, due to:
- Low digital confidence (only 9% of participants in this study felt “very comfortable” with digital tools)
- Limited understanding of the long-term benefits of exercise
- Lack of personalised, real-time monitoring tools
This project addresses these issues by targeting independently living older adults at risk of falls, and validating a real-world, tech-enabled alternative that integrates wearables, AI-driven fall risk insights, and behavioural coaching.
By working with local fall prevention teams in North and South Lanarkshire and incorporating user feedback, the project aims to supplement and scale existing services, not replace them, while empowering older adults to take greater control of their health.
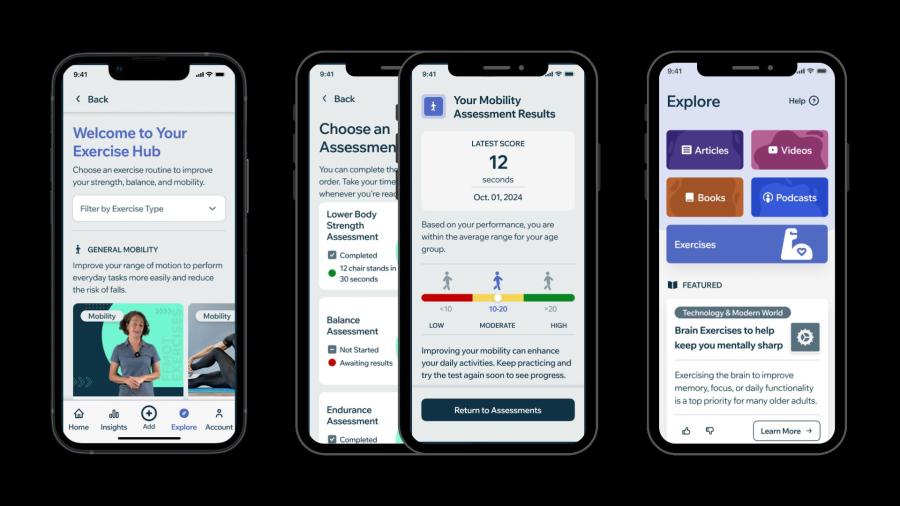
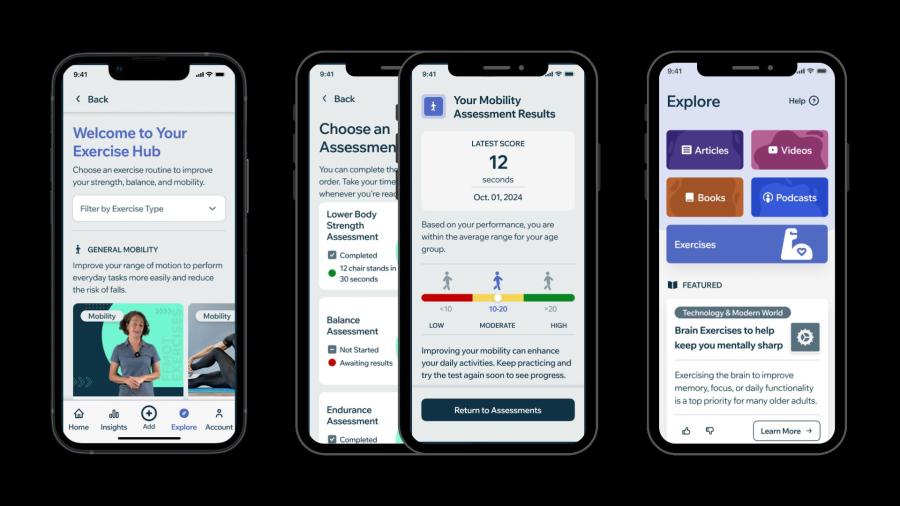
Image

What is the solution to the problem?
The solution is Smplicare’s AgeWell Coaching Platform, a digital health tool designed to empower older adults to reduce their risk of falls and improve functional wellbeing through personalised coaching, real-time monitoring, and AI-driven insights.
At its core is the Smplicare Fall Risk Algorithm (SFRa), which uses data from wearable devices (Fitbit Inspire 3) to generate fall-risk classifications based on daily step counts, sleep quality, heart rate, and other biometric metrics. The system analyses these metrics over a 15-day or 7-day window to deliver daily “fall risk” or “no fall risk” assessments.
Implementation:
The solution was tested over a four-month pilot with 35 older adults across Lanarkshire and Glasgow. Participants were onboarded through a mix of in-person and remote sessions. The app ran on iOS and Android and synced with Fitbit data using a secure API. Real-time analytics and risk scores were processed and stored on AWS cloud infrastructure, ensuring resilience and scalability.
Core
(indirectly)
Other 3rd parties
Connectivity Requirements:
The platform supports Wi-Fi, 4G and 5G connections. No private 5G network is required.
- Wi-Fi is suitable for home use (most common scenario).
- 4G/5G allows data syncing on the go but may be unreliable in older buildings (e.g., Larkhall Leisure Centre required team members to step outside for signal).
- Private 5G is not currently required due to low bandwidth usage, but could offer resilience in shared environments (e.g., care homes, housing schemes).
Energy Consumption:
The Fitbit Inspire 3 requires charging approximately once per week.
- The mobile app runs on smartphones or tablets with typical daily usage and low processing overhead.
- The solution is lightweight, requiring no additional hardware or mains-powered sensors in the home.
Key Enablers:
- Wearable sensor: Fitbit Inspire 3
- Mobile devices: Android or iOS smartphones/tablets
- Backend infrastructure: AWS with end-to-end encryption
- Daily insights: Exercise Hub, Daily Reflection, Daily Health Tip, Functional Fitness Assessments
Safety Considerations:
- All wearable and app components were tested for comfort, usability and accessibility in older adult populations
- The app complies with WCAG 2.0 accessibility standards
- Fitbit Inspire 3 previously validated in older adult trials (UKRI-funded study)
- No safety issues or incidents were reported during the pilot
- Product Integration:
- Real-time integration with Fitbit’s API
- Secure analytics and dashboard for risk scoring
- Planned integration into referral pathways with HSCPs and NHS services
- Designed to complement (not replace) in-person fall prevention classes
Image
Commercial model (Business Case)
Smplicare’s AgeWell Coaching Platform offers a scalable, cost-effective model for enhancing falls prevention services through digital delivery. It supports a shift from reactive to preventative care, providing measurable value to local authorities, HSCPs, NHS services, housing providers, and insurers.
Financial Returns / Efficiencies:
- Reduces the incidence and severity of falls, supporting cost avoidance on hospital admissions, social care, and long-term rehabilitation
- Delivers targeted support earlier, alleviating long waiting lists for in-person falls classes
- Reduces staff dependency for class delivery through self-guided app usage
- Supports evidence collection for annual programme funding reviews by enabling continuous impact reporting
Conditions to Realise Savings:
- High user engagement maintained through features like goal setting, notification prompts, engagement streaks, functional fitness progress and personalised daily action plan
- Digital onboarding and support (e.g. in-app prompts, training materials, helpline)
- Strong alignment with referral pathways to support scalable rollout
Timescales to Realise Benefits:
- Behavioural change and user engagement impact visible in 4–6 weeks (e.g. increased exercise, confidence, reduced fall worry)
- Longer-term cost savings through reduced hospitalisation and improved mobility observed over 6–12 months
- Platform readiness for rollout in Q2 2025 (via Fall Fit app version)
Estimated Market Size:
- 30% of the population over-65, nearly 4 million people
- Early target is ten leading HSCPs and ten supported housing providers in the next 18 months
Investment Options:
- Low CAPEX model: Utilises users’ own mobile devices and off-the-shelf wearables (Fitbit)
- Flexible licensing: Potential for bulk licences to HSCPs or housing providers
- Subscription model for users post-pilot, with early-adopter discounts available
Procurement Considerations:
- Smplicare has invested in achieving DTAC compliance and will be on the DSPT framework in Q2 2025
- Engaged Clinical Safety Officer, conducted penetration testing, aligned with ISO 270001 and has achieved both Cyber Essentials and ORCHA certification
Ongoing alignment with NHS Digital guidance and clinical governance practices, including accessibility, usability, and interoperability standards.
Upskilling / Support Requirements:
- Minimal upskilling required for users; app is accessible and tested with older adults
- Organisations may require light-touch onboarding and training for support staff
- Dedicated account managers planned to support regional implementation
Cost to Scale Up:
- Cost-effective at scale due to use of commercial wearables and low infrastructure costs
SFRa Fall Risk Classification for a Participant who experienced a fall during the study period
Image
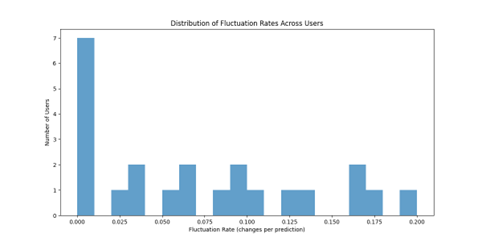
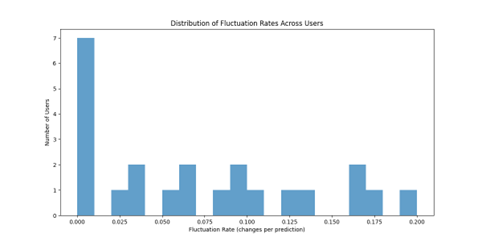
Fluctuations of the SFRa in our cohort
Image
Benefits
The pilot demonstrated that Smplicare’s AgeWell Coaching Platform delivers broad and measurable benefits across health, care, economic and digital inclusion outcomes. The app supports sustained behaviour change, improves confidence and strength, and enables a more preventative approach to falls across the system.
- Digital Inclusion
- 100% of participants completed at least one seven-day engagement streak
- 78.2% Fitbit compliance, indicating strong daily engagement
- 103 educational articles were read in-app
- The app’s interface was redesigned using WCAG 2.0 standards to improve accessibility for older users
- App available via Android and iOS
- Health & Safety
- 27% of participants felt less worried about falling after just four months
- 77.3% reported feeling more motivated to stay active
- 95.4% improved understanding of the role of exercise in maintaining independence
- 63.6% felt physically stronger
- Functional fitness tests showed gains in endurance (+25 steps) and strength (+4.6 sit-to-stand repetitions)
- Economic & Efficiency
- Reduces pressure on NHS and social care services through fewer fall-related incidents
- Shortens waiting times by supporting earlier intervention for those awaiting in-person support
- Captures robust data to support annual funding reviews and evidence value for money
- Enables a hybrid model: digital first, in-person where needed — optimising practitioner time
- Energy & Environmental
- Platform runs on low-energy consumer wearables with no additional infrastructure
- Encourages home-based exercise, reducing transport and site energy use
- Minimises waste by using existing devices and networks
- Comfort, Confidence & Independence
- 71.4% of users entered the study worried about falling 27% felt less anxious by the end
- 73% completed daily reflections and built healthy routines
- 50% reported greater flexibility and independence when walking
- High confidence using the app: 73% felt comfortable exercising independently with video guidance
- Quotes highlight users “went to football without a stick for the first time in years” and exercised “more than they normally would”
- Social & System-Level Benefits
- Complements and strengthens existing falls pathways
- Enables local authorities and HSCPs to offer scalable solutions without overloading staff
- Opens opportunities for data-driven planning and preventative investment
- Can be adapted to support wider healthy ageing outcomes, including frailty management and physical literacy
Respondents feedback…
“The exercises are already helping me get my confidence back. This weekend, I went to the football without my stick for the first time in a long while.”
Respondent 17 Feedback
“I have learnt more about my personal physical and mental health and how much it affects my life daily.”
Respondent 21 Feedback
“The Smplicare app changed my view on how to exercise. It motivated me to go out and make sure I did not just sit about.”
Respondent 18 Feedback
Practitioner feedback
“We often have a bottleneck of referrals, causing waiting lists. Something like this for our organisation could open this up to those who are on waiting lists or are unable to travel to our in-person sessions.”
Practitioner 1 Feedback
“A solution like this can provide the evidence that doing physical activity will save money to the NHS, demonstrating our impact and allowing us to continue investing in our programmes.”
Practitioner 1 Feedback
“This would be an activity coordinator's dream. They’d love something like this to facilitate activities.”
Practitioner 4 Feedback
Lessons Learnt
This pilot delivered clear insight into how to successfully implement and scale a connected care falls prevention solution with older adults. The project highlighted the importance of user engagement, co-design, and flexible implementation.
Do’s
- Engage early and often with both users and practitioners to co-design features and pathways
- Provide in-person onboarding where possible to build user confidence and digital trust
- Incorporate motivational features (e.g. daily reflection, goal setting) to support long-term engagement
- Develop fallback models, like a 7-day algorithm, to accommodate real-world data gaps
- Design for accessibility, WCAG 2.0 standards ensured app use was inclusive and intuitive
- Build flexibility into project budgets and delivery, reallocation via Project Change Requests enabled faster response to changing needs
Don’ts
- Don’t assume all older adults are digitally confident, only 9% felt “very comfortable” with tech
- Don’t rely solely on online content, hands-on training and helplines remain critical
- Don’t enforce rigid usage patterns – allowing natural interaction gave a clearer picture of usability
- Don’t overlook the importance of local connectivity, e.g. poor 4G/5G indoors delayed onboarding in community settings
- Don’t under-resource compliance, public sector procurement required additional investment in DTAC, DSPT, and Clinical Safety processes
Previous experience / Best practice guidance
Fitbit Inspire 3 was previously validated for older adults in a UKRI-funded study, improving adoption confidence
- In-person classes remain essential, digital should supplement, not replace them
- Waiting lists and referral bottlenecks can be eased by offering digital-first access, with practitioner support layered on
- Building in feedback loops (e.g. co-design sessions, surveys, interviews) ensures continuous improvement
- Parallel workstreams and a multi-disciplinary team (data, UX, clinical, technical) helped the team remain agile and responsive